Introduction
Skull base is provided with many important foramina which gives passage to multiple important neurovascular structures, entering into the cranial cavity from extracranial regions or passing through the foramina to exterior. In middle cranial fossa there are 3 such foramina which are persistently present at the junction of body and greater wing of sphenoid-foramen rotundum, for amen ovale, foramen spinosum. Because their clinical implications are more, so we studied the foramen ovale and foramen spinosum on morphometric ground on 76 cases. Posterior to superior orbital fissure there is foramen rotundum which convey s the maxillary division of trigeminal nerve. Posterolateral to the foramen rotundum is foramen ovale, which is largest among all the foramina present in middle cranial fossa and transmits mandibular division of trigeminal nerve along wit h accessory meningeal branch of maxillary artery, lesser petrosal nerve and an emissary vein connecting the pterygoid venous plexus in the infratemporal fossa to the cavernous sinus.1
Foramen ovale is generally oval in shape but variations are present also, and it is used in different diagnostic and therapeutic procedures by neurosurgeons. Ossification of sphenoid starts from its greater wing (alisphenoid) in membranous centre and during ossification foramen ovale develops surrounding the mandibular nerve.
At the junction of posterior border and lateral border of greater wing of sphenoid, near the root of the spine of sphenoid, the foramen spinosum is p resent. Middle meningeal artery, commonly involved in epidural haemorrhage, enters through the foramen spinosum. For amen spinosum may be duplicated, giving passage to two divisions of middle meningeal artery separately. Foramen spinosum may be absent as previously reported by many authors. Observations of these foramina will be helpful for different surgical interventions as well as for diagnostic procedures.
Materials and Methods
A morphometric study was conducted on foramen ovale and foramen spinosu m in the department of Anatomy, Medical college Kolkata. A total of 38 specimens (36 human skulls & 2 sphenoids) were studied and dimensions (length & width) of foramen ovale were measured using digital caliper. We aslo observed for the shape of foramen ovale and noted down the variations. Photographs were taken by digital camera. Damaged skulls were excluded for this study. Different types of variations, that were obtained, were tabulated by using appropriate charts and graphs separately and statistical analysis observing the relevant norms done to show significance of finding.
Results and Discussion
A study was conducted on 36 human skulls & 2 sphenoid bones. Totally 38 specimens were studied. We found most common sh ape of foramen ovale was of oval type and was present in 53.94% cases. The shape of foramen ovale was round in 21.05% cases, almond in 21.05% cases and D-Shaped in 3.94% cases. In 3 out of 76 cases (3.94%) there was bony spicule within the foramen. The maximum length and width of foramen ovale on the right and left side was 8.26 mm, 4.58 mm and 10.71mm, 5.17 mm respectively. Minimum length and width of foramen ovale on right and left side was 6.25 mm, 2.37 mm and 5.80 mm and 2.28 mm respectively. Mean length on right and left side was 7.17 mm and 7.26 mm and mean width on right and left side was 3.49 mm and 3.73 mm respectively.
Foramen spinosum was absent in one case, where foramen spinosum was confluent with foramen ovale.
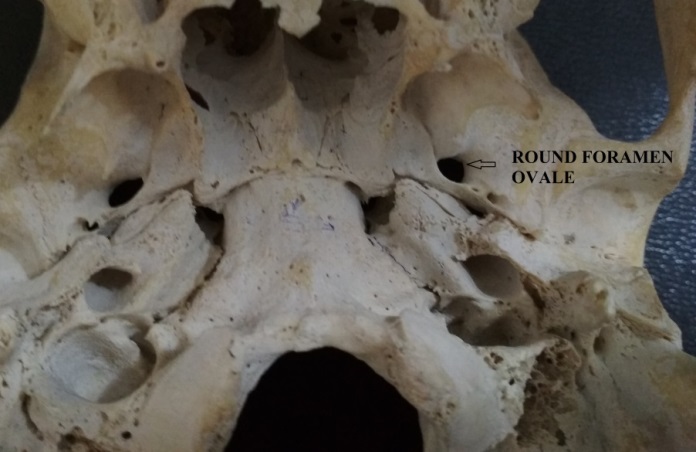
Figure 1
Photograph of base of skull showing almond shaped right foramen ovale and oval shaped left foramen ovale.

Figure 3
Photograph of base of skull showing left foramen ovale is oval in shape and a bony spicule is projecting within the foramen ovale.

Figure 4
Photograph of inferior surface of sphenoid showing D-Shaped left foramen ovale with a spicule projecting into foramen ovale in same side.

Table 1
| Shape | Right (n=38) | Left (n=38) | Total (n=76) |
| Oval | 22(57.9%) | 19 (50%) | 41 (53.94%) |
| Round | 6 (15.8%) | 10 (26.3%) | 16 (21.05%) |
| Almond | 8 (21%) | 8(21%) | 16 (21.05%) |
| D-Shaped | 2 (5.3 %) | 1(2.6%) | 3 (3.94% ) |
Distribution of cases according to shape of foramen ovale
Table 2
Distribution of cases according to length & width of foramen ovale
Transcutaneous approach of Gasserian ganglion for surgical intervention of trigeminal neuralgia which is performed through foramen ovale makes the foramen significant for assessment regarding its shape and dimentions. Current trends toward percutaneous biopsy of cavernous sinus tumor through foramen ovale2 and placing electrode in foramen ovale for evaluating seizures in patients who undergone amygdalohippocampectomy3 has increased the risk of mandibular nerve injury to some extent. Moreover inadvertent injuries to Mandibular division of trigeminal nerve during different neurosurgical procedures can result in varied and grave symptoms. Inspite of increasing microsurgical techniques and their considerable surgical importance, there are not many studies on skull base foramina from this part of India. Stenosis or presence of a bony spicule within the foramen ovale may result compression effect over mandibular nerve producing different clinical symptoms.
Table 3
Comparison between previous studies and present study
Higher incidence of oval type of foramen ovale was reported by most of the authors. In our study we also found that the most common type of foramen ovale was of oval type and was present in 53.94% cases, followed by round in 21.05%, almond in 21.05 % cases and D-shaped in 3.94% cases. In their study Ray5 and John Anna Deepti9 founds it shaped foramen ovale in 1.42% and 1.67% cases respectively. But we didn’t find any such and our least common type was D-shaped, similar to the finding of Kumar Binod.4 In 3 out of 78 cases (3.84%) we found bony spicule projecting within foramen ovale. But Biswabina Roy5 and John Anna9 found projections within the foramen ovale in different forms, spine, tubercle, bony bar or bony plate in 24.2% and 31.66% cases respectively, which is much higher in respect to our study. Presence of a bony bar or plate within the foramen ovale can completely devide the foramen into two or more compartments. Such findings were recorded by Poornima B et. al,10 who found duplication of foramen ovale in one skull among 200 specimens. Ray B, Reymond et. al11 also found compartmentalised foramen ovale. G Karthikeyan et. al7 conducted a morphometr ic study on 64 dry adult skulls. They found similar type septation within the foramen ovale by a thin bony plate. In another skull, they found ossified pterygospinous ligament passed just inferior to left foramen ovale, deviding the foramen into compartments.
Biswabina Ray5 et. al conducted a morphometric study in the Department of Anatomy, Manipal College of Medical Sciences, Pokhara, Nepal. They concluded that mean length of foramen ovale is 7.46 + 1.41 mm and 7.01+ 1.41 mm on right and left side respectively. In our study the mean length of foramen ovale was closer to the findings of Ray5 and Rao Sadananda.6
According to a study conducted by Kumar Binod4 et al in the Department of Anatomy and Forensic Medicine at IGIMS, Patna and other Medical Colleges of Bihar, mean length of foramen ovale on right and left side was 6.86 + 1.26 mm and 6.84 + 1.3 mm respectively. The maximum length of foramen ovale on right and left side was 10 mm and 9.8 mm and minimum length of foramen ovale on right and left side was 4.4 mm and 3.4 mm respectively. Both the values are few mm greater in our study.
Foramen spinosum may be absent in one side or both. Studies on skull base foramina previously conducted by other authors have revealed about existence of such cases where foramen spinosum was present only in one side. Bergman12 observed such finding in 1% case. If the foramen spinosum is absent in one side, there is high chance that the middle meningeal artery which usually passes through foramen spinosum will enter the middle cranial fossa through foramen ovale. In our study we found a case of unilateral foramen spinosum where foramen spinosum was confluent with foramen ovale on left side of skull base.
Conclusion
Mandibualr division of trigeminal nerve passes through the foramen ovale, so any spicule or bony plate present within foramen ovale will produce compression effect over the nerve and such bony spicule or plate may also create interference during different operative procedures through this route. Knowledge about the variations of these foramina will help the clinicians during different diagnostic and surgical procedures. In different microsurgical techniques foramen spinosum is used as landmark. Knowledge about the variations of foramen spinosum will help the neurosurgeons also.12